One challenge that designers face is creating a physical form factor that can be comfortably attached to the body for months at a time. In this case, the solution was to make a two-part system. The coin-sized sensor unit attaches to the user’s body with a biocompatible adhesive patch. The hand-held reader unit analyses the data and allows the user to transfer that data to medical professionals for further analysis. This functional partitioning enables the body-worn sensor to be as small and light as possible. A block diagram of the monitor’s sensor and reader is shown in Fig. 3.
Another challenge is to anticipate all of the environments that the user will be in, and the activities in which she might engage. With a usage time frame of months, a wearable device must accommodate a wide range of conditions including sleeping, exercising and showering. In this case, the design of the sensor and its packaging had to enable precise temperature measurements regardless of whether the sensor is open on one side or covered by the user’s arm.
The designers solved this problem by using a pair of matched thermistors. These measure the temperature and the heat flow from one side of the sensor to the other, making the sensor accurate to a few thousandths of a degree. In addition, the user’s movement is taken into account by incorporating an accelerometer in the sensor design.
Body-worn electronics has to be very small, which means the volume available for batteries is limited. So another challenge of the sensor design is to keep the power consumption extremely low. The designers of this sensor used an 8-bit microcontroller in order to minimise the sensor’s cur-rent consumption. Minimal current consumption was achieved by using the microcontroller’s ultra-low-power wake-up feature.
When it’s time to take a reading, the sensor powers up, takes a measurement and then returns to sleep mode—all in less than one millisecond. This short wake-up time enabled the device designers to achieve average power consumption of less than 1 μA and a battery life of six months using a small CR1216 lithium coin cell battery.
Another challenge is to transfer the measured data. This sensor module sends data to the reader using a modified radio frequency identification (RFID) protocol, wherein communication is initiated by holding the reader near the sensor. This data transfer requires higher power consumption than that required for measuring the data. So the designers minimised the current drawn by holding the sensor’s temperature readings in 16-megabytes of standalone Flash. This allows reader data uploads to be spaced a few days apart.
Since the data collected by a long-term sensor may need to be analysed by a trained person, creating a straightforward and cost-effective way to transfer the measured data to a PC and communicate over the Internet is yet another important design consideration. The second part of this device—the handheld reader—is utilised for this purpose.
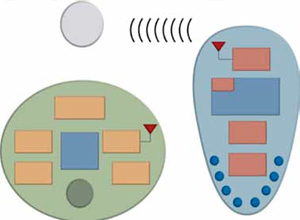
The reader transfers the data to a PC via the on-chip USB peripheral inside a 16-bit microcontroller with nanoWatt technology. The user can enter additional data via front-panel buttons that are implemented using the microcontroller’s internal charge time measurement unit and mTouch capacitive-touch technology.
Communication from the device manufacturer to the reader allows for refinement of the ovulation pre-diction. The same capability can allow remote reconfiguration of the microcontroller. With this flexibility, the manufacturer can run diagnostics and send software updates to the monitoring system.
As innovation continues in the fields of biology, physiology, chemistry and electronics, wearable medical devices that are meant for long-term use will create new diagnostic and therapeutic options for even more illnesses and conditions.
The author is a staff engineer in medical products group of Microchip Technology Inc.