UC San Diego and Boston University researchers develop a breakthrough optical biosensor for faster and affordable monkeypox detection.
In a significant advancement in viral diagnostics, researchers at the University of California San Diego School of Medicine, alongside collaborators from Boston University, have introduced an optical biosensor that swiftly identifies monkeypox, the virus behind ‘Mpox’. This innovation marks a pivotal shift in diagnostic technology by eliminating the dependence on conventional laboratory setups.
Monkeypox symptoms, such as fever, lesions, and rashes, often mimic those of other viral infections, making visual diagnosis unreliable. “So just by looking at the patient, it is not easy for clinicians to distinguish monkeypox from these other diseases,” said Partha Ray, co-principal investigator and associate project scientist, UC San Diego. Current diagnostic methods like polymerase chain reaction (PCR) are both costly and time-intensive, posing challenges during outbreaks. The biosensor addresses this limitation with its rapid, cost-effective diagnostic process, a vital tool amid global health emergencies.
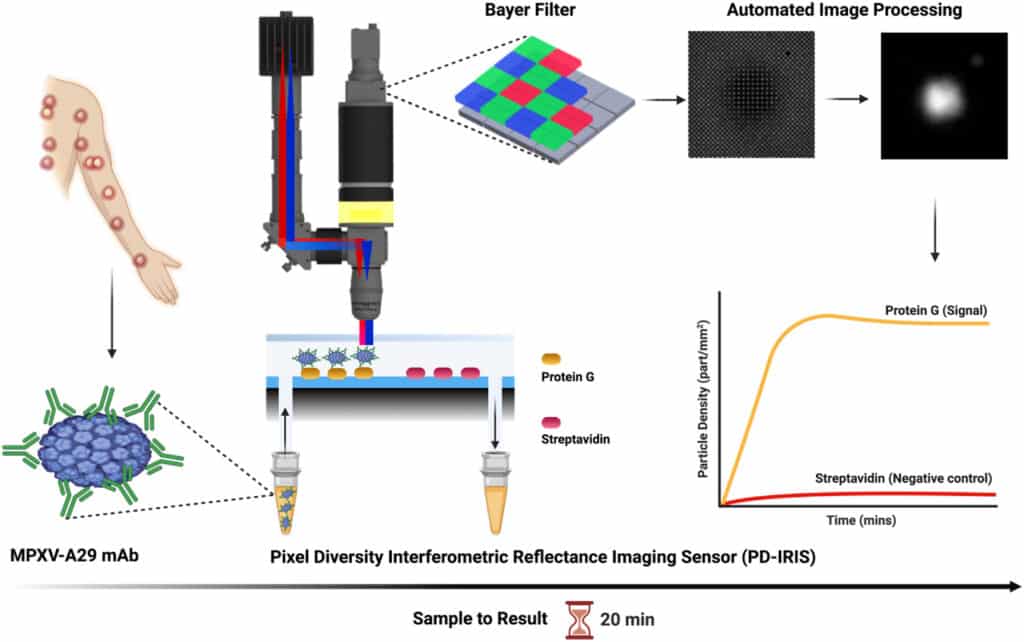
Central to this biosensor is a sophisticated platform known as pixel-diversity interferometric reflectance imaging sensor (PD-IRIS). Developed by Boston University’s Professor Selim Ünlü over years of research, this technology employs silicon chips that interact with viral proteins through monoclonal antibodies. These antibodies, prepared by Ray’s team, bind to the virus in patient samples. When exposed to light, the chips generate interference patterns that reveal the presence of the virus with high sensitivity.
Remarkably, the biosensor can differentiate monkeypox from other clinically similar viruses, including cowpox and herpes simplex, within minutes. “Within two minutes, we can tell whether someone has monkeypox or not,” noted Ray. From sample collection to diagnosis, the entire procedure takes about 20 minutes, a significant improvement over existing methods.
Designed for scalability, the biosensor could be adapted for diagnosing other viruses, such as HIV or syphilis, by altering the antibodies used. Mass production of diagnostic kits is being explored, though government support is essential for widespread implementation. Ray emphasised the urgency, stating, “If we don’t take care of this particular epidemic right now, it is not going to be limited within Africa.”
This rapid, adaptable diagnostic tool is poised to transform viral outbreak management, offering hope for containing future pandemics effectively.