The introduction of artificial pancreas (AP) has proved to be a boon for diabetic patients. This medical device has the potential to improve the conditions of people infected with type 1 diabetes (T1D). Hence, people must be aware of the working of AP in order to utilise it for maximum health benefits
Diabetes mellitus (commonly known as Diabetes) is one of the serious chronic diseases characterised by high glucose levels in the blood. The main cause of this disease is the inappropriate working of the organ called pancreas. This disease affects the ability of the body to produce or use insulin appropriately.
The pancreas is located in the abdomen behind the stomach. When we eat food, our body converts that food into energy through glucose. Therefore after a meal, when the glucose level in the blood increases, beta cells of the pancreas release insulin, which stimulates fat cells to remove excess glucose from the blood and stores it in the liver in the form of glycogen, thereby maintaining blood glucose level in the desirable range of 70mg/dL to 180mg/dL.
When the concentration of glucose in the blood gets low, alpha cells of the pancreas secrete hormone called glucagon by catabolising glycogen stored in the liver. The blood sugar level of a diabetic patient thus remains normal. The glucose drop might be due to insulin not being produced in the appropriate amount as it should be.
As per the International Diabetes Federation, 415 million individuals suffered from diabetes in 2015, and it is estimated that 642 million people within the age group of 20 to 79 years will suffer from this disease by 2040. Diabetes leads to adult blindness, end-stage renal disease and viral infections, cardiovascular diseases, cancer, and injuries. It is considered as the fifth main cause of worldwide death. Individuals with diabetes are susceptible to coronary illness as well.
Generally, there are two types of diabetes: Type 1 diabetes (T1D) and type 2 diabetes (T2D). In T1D, the immune system gets damaged and attacks beta cells in the islets of Langerhans of the pancreas that release insulin. Due to this, individuals infected with T1D need daily injections of insulin to survive.
Whereas in T2D, the body makes enough insulin but is unable to utilise it effectively. Adults above the age of forty years usually get infected with T2D.
Gestational diabetes is a type of diabetes that happens in pregnancy and normally vanishes when the pregnancy is over. Ladies who suffer from gestational diabetes are prone to develop T2D later in life.
The medical practitioners and healthcare researchers have taken various steps to tackle the problem of diabetes, such as the development of a mathematical model of glucose-insulin dynamics, automatic infusion pumps, sensors to monitor glucose level, and a control system for automatic infusion of insulin.
By using new technologies in glucose monitoring and insulin infusion rate, it is possible to sense the glucose level by using continuous measurements of glucose monitoring. The industrial and scientific community has been increasing its efforts to develop and replicate the technological phenomenon of the pancreas through artificial pancreas (AP) to control insulin delivery.
What is artificial pancreas?
Artificial pancreas is a man-made scientific technology developed in order to match the working of the pancreas. It is designed to change glucose levels in the bloodstream in a similar way as the human pancreas does throughout the day and overnight.
Maintaining a balanced glucose level is important for the proper functioning of brain, kidney, and liver. Therefore it is important for T1D patients to maintain these levels when the body cannot produce insulin.
An AP system consists of three devices—an insulin delivery pump, a continuous glucose monitoring system (CGM), and a computer-controlled algorithm in order to allow real-time communication between two devices. The AP system is sometimes referred to as a closed-loop device as the patient is not in the decision-making loop, or an automatic system for glucose control.
After monitoring the blood glucose levels, the AP system manipulates insulin infusion pump rates by a closed-loop controller that receives information from the sensor in order to reduce the incidence of low blood glucose due to the over administration of insulin (hypoglycemia) and high blood sugar due to failure of enough administration of insulin or high-intensity exercise (hyperglycemia). Hypoglycemia is a short-term risk that results in drowsiness, shakiness, and even loss of consciousness. Hyperglycemia is a long-term risk that results in blindness (diabetic retinopathy), numbness (diabetic neuropathy), and kidney failure (diabetic nephropathy).
Researchers are currently working on three main types of artificial pancreas:
- Closed-loop artificial pancreas. Closed-loop artificial pancreas is also called a closed-loop insulin system in which an insulin pump communicates wirelessly with a CGM inserted under the skin. The CGM measures blood sugar concentrations in patient cells and sends the result to a small computer where the control algorithm analyses the result and calculates the correct insulin dosage.
- Bionic pancreas. Bionic pancreas is being developed by Dr Edward Damiano’s Beta Bionics firm. It consists of two pumps that deliver insulin and glucagon, respectively, and automatically controls blood glucose levels. The pump is wirelessly connected to the iPhone that enables real-time communication between devices and calculates the required insulin or glucagon doses.
- Implanted AP. Developed by researchers of De Montfort University, the implanted pancreas contains a gel that acts according to the changes in glucose level. The gel administers a higher dose of insulin if the concentration of glucose increases and decreases the amount of insulin during low glucose concentration. It can be refilled with insulin consistently.
According to researchers, the closed-loop system of blood glucose regulation reduces the risk of hypoglycemia in adults.
How artificial pancreas works?
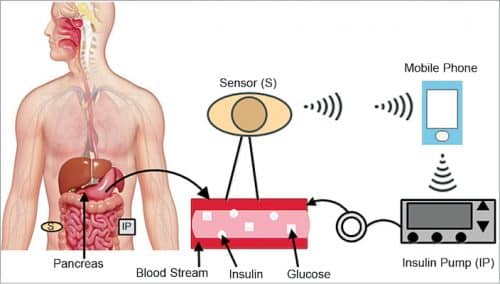
The complete AP model is shown in Fig. 1, with its major operation described in Fig. 2. The AP comprises following units:
CGM
A CGM takes ongoing blood glucose readings through a little sensor inserted into the skin and maintains a stable flow of information about diabetic patient glucose levels in the bloodstream. A sensor that is fitted under the patient’s skin (subcutaneously) continuously monitors the concentration of glucose in the blood around cells. A small transmitter sends data to the receiver. CGM provides a continuous display of estimates of both blood glucose levels and direction and rate of change of these estimates. To get the correct predictions of blood glucose from a CGM, the diabetic infected patient needs to calibrate the CGM periodically using measurements of glucose from a blood glucose device.
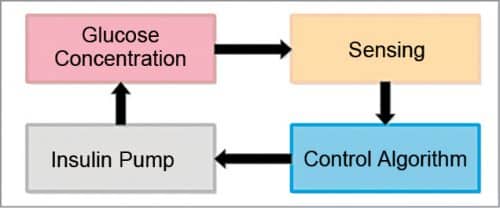
Control algorithm
A computer model or controlled algorithm embedded in an external processor, also called the controller, performs a series of mathematical calculations after receiving information from a CGM. The controller manipulates the insulin infusion rate based on these calculations.
Insulin pump
It injects the correct dosage of insulin to the fatty tissue below the skin according to the instructions sent by the control algorithm. As a result, insulin moves throughout the bloodstream, thus lowering blood glucose levels.
Patients
Patients are a significant part of the AP system. The amount of glucose in the bloodstream frequently changes as it gets affected by food taken by the patient, intensity of physical activity, and other substances.
Current international trends
Artificial pancreas device based on technology from the University of Virginia, Center for Diabetes Technology has been accepted by the US FDA (Food and Drug Administration).
This device, also called Control-IQ, automatically injects the required dosage of insulin to patients with T1D. It is manufactured by Tandem Diabetes Care that monitors glucose levels with Dexcom G6 CGM. People using this system are free from checking blood glucose levels frequently in a day by fingerstick and also from the delivery of insulin by injections multiples time a day.
The Omnipod Horizon System announced the successful trials of their AP system that uses a tubeless patch pump instead of a regular tubed one. It is the most recent Dexcom CGM technology, an improved version of insulet’s handheld controller. This system provides the same satisfaction as the present omnipod system, such as a non-stop dosage of insulin and refrains from delaying insulin dosage during exercising or other physical activity.
Researchers are now focusing on the Internet of Things (IoT) devices in order to implement them in the healthcare industry. OpenAPS (artificial pancreas system) initiative was built for a diabetic patient to have a smarter way of blood glucose monitoring and controlling the levels rather than waiting for a new system. Patients are able to feed data of CGM in order to give information to software about glucose levels.
With OpenAPS, a piece of hardware is used that communicates with the pump to get past values of dosage and adjust the required insulin supply. Many patients are having the benefits of software by downloading it online. OpenAPS has built a subdermal system that communicates with a smartphone to provide glucose level information and a vibrating module (alarms) that alerts diabetic patients when glucose levels are above or below the threshold values.
FDA also approves Medtronic AP for diabetic patients over fourteen years. The device named MiniMed 670G is referred to as a hybrid closed-loop system that monitors glucose levels after every five minutes and administers insulin when needed. The system is ‘first-of-its-kind technology’ that combines insulin pumps and glucose monitors in one device.
Now FDA has accepted to cover 7 to 13-year-olds as well. There is advancement in T1D with the development of Zynquist (sotagliflozin) by Sanofi and Lexicon Pharmaceuticals. It is the first oral antidiabetes medication for T1D patients that inhibits SGLT-1 and SGLT-2 (sodium-glucose cotransporter types 1 and 2). SGLT1 manages the glucose absorption in the gastrointestinal tract, whereas SGLT2 is responsible for glucose reabsorption by the kidney.
Zynquist provides important benefits to adults with T1D by reducing blood sugar reabsorption in the kidneys through SGLT2 inhibition and delaying blood sugar absorption through local SGLT1 inhibition in the intestinal tract.
Researchers from Canada are working on doubling up hormone, which can increase the time spent in the target glucose range to 86 per cent, according to trials on AP. The team delivered two hormones, that is, pramlintide alongside insulin to have better glucose management after diet for T1D patients. The pancreas makes the hormone amylin after meals to manage glucose levels, and pramlintide is a man-made version of amylin. People infected with T1D disease do not have usual amylin release, and so this dual-hormone AP system is used to alter glucose levels.
The worldwide AP market has been divided based on the following factors:
By the method of type
It contains systems like threshold suspend device system, non-threshold suspend device system, control-to-target system, and control-to-range system. When the patient is not responding to threshold alarms, these devices take an immediate control action.
By mode of treatment type
It involves a hybrid closed loop, bi-hormonal, and insulin.
By mode of end-use
It includes clinics, research, hospitals, and others.
Current status in India
As per the International Diabetes Foundation, India has the highest number of diabetic patients in the world. This disease has its impact on more than fifty million Indians and kills about one million patients every year. This big frequency is a result of the sluggish lifestyle and consumption of high-calorie diet by the growing middle class. So, in order to combat diabetes, various scientific institutions in India are doing efforts to develop AP.
Indian Institute of Science (IISc), Bengaluru, has developed an artificial pancreas to treat T1D. The scientists and researchers are working together with specialists at the MS Ramaiah Medical Hospital to design the pancreas system. The Ministry of Human Resource Development (MHRD) and the Indian Council of Medical Research (ICMR) have given 36 million rupees for the project.
The Narayana Multispecialty Hospital in Hyderabad is the first hospital that provides artificial pancreas treatment. Each session of treatment procedure costs around 4,000 rupees, and a minimum of ten sessions are required to see improvement.
IIT Mumbai has developed a bioartificial pancreas that can be implanted in diabetic patients to treat diabetes. It has been successfully tested on mice and pigs. The bioartificial pancreas device has been developed utilising the polymer-based hollow fibre, which will be fitted near the pancreas in the abdominal muscles. It can develop cells that secrete insulin.
Opportunities for electronics and computer science engineers
IoT has transformed the field of electronics engineering. IoT has various applications, especially in the healthcare industry. With the help of IoT, engineers can send real-time data of concentrations of blood glucose to a number of devices they want to connect, such as from an Android phone to an iPad or smartwatch that makes day-to-day monitoring of diabetes easy.
The interest and development in AI have been increasing in the healthcare industry over the past decades. Engineers can apply various methods of AI in the management of diabetes and predict the risk of diabetic complications. Machine learning (ML) methods used in food recognition applications can help patients with T1D to have more correct choices of food and insulin management decisions. By using deep learning methods, engineers are able to have a more accurate estimation of blood glucose levels and detect the stage of hypoglycemia.
Conclusion
The innovation of AP has proved to be a boon for diabetic patients and opened a new field of research for the electronics and computer engineering domain. This medical device has the potential to bring peace of mind to more than one million people infected with T1D. We need to make this device available to all the people who are infected with diabetes and make sure that this technology is flexible enough to use in the real world to achieve the best outcomes.
Other thrilling advances include the development of autonomous systems that not only monitor insulin but also glucagon (which raises blood sugar level) in order to have complete control over sugar levels.
Krishma Prashar is currently pursuing her ME degree in Electronic Instrumentation and Control Engineering from Thapar Institute of Engineering and Technology, Punjab. Her research interests include control systems, biomedical engineering, and industrial automation
Sahaj Saxena is currently working as an assistant professor at the Electrical and Instrumentation Engineering Department of Thapar Institute of Engineering and Technology, Punjab. His main area of research is biomedical control systems



This is great. It will save lives.
Thank you for your feedbaack.
i love this can i just say the innovation behind this is amazing good work
Thank you for your valuable feeback.