Three facets of personal healthcare—gait- and posture-related disorders, geriatric care and treatment of neurodegenerative disorders—are set to see important changes, driven by the emergence of sensors-laden smartphones as the centerpiece of democratisation of healthcare hardware.
On a balmy mid-April afternoon, amidst the cacophony of passionate deliberations ringing the walls of Paul Brest Hall on Stanford University’s sylvan green campus, a picture began to emerge. It was the annual mHealth Connect conference. Most of the talks by academic stalwarts, healthcare entrepreneurs and venture capitalists were harping on a common thesis, “The growing nexus between mobile sensors and artificial intelligence (AI) in the healthcare domain.”
Amidst ardent calls for Silicon Valley-styled disruption of the ailing healthcare sector, it became ostensibly clear that three facets of personal healthcare were going to see important changes, driven by the emergence of sensors-laden smartphones as the centerpiece of democratisation of healthcare hardware. In the next few paragraphs you will be exposed to the following three domains earmarked to be the recipients of the disruption: gait- and posture-related disorders, geriatric care and treatment of neurodegenerative disorders (Parkinson’s disease, multiple sclerosis, Alzheimer’s disease and Huntington disease).
At first glance it might seem as if ushering these advancements demands dramatic popularisation of highly-specialised and potentially expensive medical sensors, such as photo-plethysmo-gram (PPG) heart rate monitor sensor found thus far only in high-end phones such as Samsung S8. Far from it, we will see that many solutions catering to a wide array of challenges in all three above-mentioned domains, will, in fact, be fuelled by the data emanating from the humble triad of inertial measurement unit sensors, or motion sensors, that is, accelerometers, gyroscopes and magnetometers.
With this background, let us dive deeper into the specific domains and the success stories that have emerged.
Gait- and posture-related disorders
Paleoanthropologists (those who study fossil hominids) believe that approximately four million years ago, the now-extinct hominin Australopithecus afarensis finally mastered the art of performing a series of complicated, cooperative and coordinated manipulation of the musculoskeletal and locomotor controller systems, resulting in a physical activity that we now take for granted—the upright human bipedal walk!
The repetitive pattern spanning two successive steps or one complete stride constitutes what is formally studied as a gait cycle. A gait cycle begins when the heel of one foot strikes the ground and culminates the instant when the same foot makes contact with the ground again.
As per Rancho Los Amigos system, a single gait cycle consists of eight temporal phases, which include initial contact, loading response, mid-stance, terminal stance, pre-swing, initial swing, mid-swing and late-swing phases.
Fine grained analysis of gait reveals an astonishing array of clues about a person’s state of general health, both from the orthopedic as well as the neuromuscular perspective.
From an orthopedic viewpoint, study of gait kinematic deviations from the normative model is an integral part of diagnosis of conditions such as developmental dysplasia of the hip (DDH), hip fracture and chronic ankle instability.
Stanford Motion and Gait-Analysis Laboratory lists eight basic pathological gaits that can be attributed to neurological conditions. These are hemiplegic, spastic diplegic, neuropathic, myopathic, Parkinsonian, choreiform, ataxic (cerebellar) and sensory.
A typical gait analysis study entails a physical exam, followed by video analysis and possibly electromyographic (EMG) measurements of muscle activity during movement. Enter the scene, motion sensors!
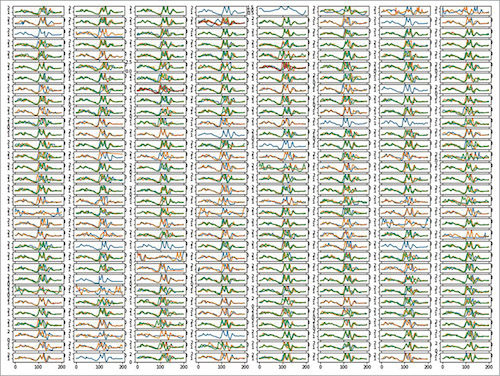
Modern-day smartphone sensors, such as accelerometers and gyroscopes, allow sampling rates of as high as 400 samples/sec. These facilitate highly precise measurements of the gait cycle that can be done by the patient just by placing the phone in his/her pocket and walking in the comfort of his/her home.
In the figure, we see a visualisation of gait cycle time-series signals measured from the accelerometer of a smartphone carried by a volunteer at UnifyID labs.
As for the question of these measurements meeting the rigour of a proper medical examination, there exists a plethora of peer-reviewed published research that showcases that it is indeed the case.
Nearly eight years ago, Rigoberto et al presented a study that showcased how they had successfully used an off-the-shelf commercial smartphone as a tool to evaluate anticipatory postural adjustments before the beginning of normal gait in healthy subjects.
In the same year, Lemoyne et al demonstrated an implementation of an iPhone as a wireless accelerometer for rigourously quantifying gait characteristics.
Then, in 2012, Nishiguchi et al studied in detail the reliability and validity of gait analysis by Xperia SO-01B Android smartphone on 30 subjects. The scientists concluded that smartphone-based measurements indeed had the capacity to quantify gait parameters with a comparable degree of accuracy that was attained using a dedicated medical grade tri-axial accelerometeric sensor.
In 2016, we saw the first usage of a smartphone as a wireless gyroscopic platform for quantifying reduced arm swing in hemiplegie gait.
More recently, researchers from Toho university have developed Gait-Kun system. It consists of tri-axial accelerometers and shows promising levels of accuracy in measuring ataxia due to spino-cerebellar degeneration.
Geriatric care
A crucial component of delivering geriatric care is continuous monitoring. In this regard, the motion sensor-laden smartphone emerges as a key tool that can be used in lieu of, or in conjunction with, video monitoring systems.
One often-ignored facet of geriatric care is fall detection and response. As stated in a study on smartphone-based fall detection systems by Stefano Abbate et al, “A fall also has dramatic psychological consequences, since it drastically reduces the self-confidence and independence of affected people. This may contribute to future falls with more serious outcomes, or it may lead to a decline in health.”
In 2012, He et al showcased how fall detection using smartphone motion sensors can be performed rather accurately, and how this technology can be a crucial piece in dramatically reducing the response time of healthcare professionals in the event of a fall.
In the same year, Fontecha et al demonstrated a system that could support physicians to construct a highly granular and centralised elderly frailty diagnosis, by munging activity data from an accelerometer-enabled cellphone with clinical data emanating from lab tests.
Besides this, Timed-Up-and-Go (TUG) test, which is also heavily used in geriatric care and for assessing the quality of recovery from hip fractures and cerebro-vascular accidents, can be performed with high accuracy using motion sensors on a smartphone.
In 2012, Mellone et al published a detailed study on the validity of a smartphone-based instrumented TUG test.
This was followed by another highly-cited work by Milosevic et al published in 2013, where the scientists introduced a smartphone application called sTUG that could completely automate the TUG test, so it could be performed by the patients themselves from the comfort of their homes.
Neurodegenerative disorders
Advancements in TUG test explored above are also applicable to neurodegenerative disorders. TUG test was initially designed for elderly persons, but is today also prescribed for patients with neurodegenerative disorders such as Parkinson’s disease, multiple sclerosis, Alzheimer’s disease and Huntington disease.
Besides this, there exists a fairly vast body of work where researchers have used motion sensors to help diagnose and assess neurodegenerative disorders. The first mobile gait analysis for early diagnosis and therapy monitoring in Parkinson’s disease was published in 2011 by a group of German researchers at University Hospital of Erlangen.
Then, in 2012, Chung et al showcased how their stride detection algorithm, when applied to accelerometric data from commercial smartphones, could be used to perform early onset detection of Alzheimer’s disease. This is based on the crucial observation that Alzheimer’s patients exhibit a significantly shorter mean stride length and slower mean gait speed than those with healthy controls. Both of these metrics could be precisely estimated using commercially-available accelerometers.
In 2014, a Taiwanese team led by Kun-Chan Lan showcased how their pedestrian dead reckoning-based gait monitoring system could be used for the early diagnosis of Parkinson’s disease.
This was followed by Kostikis et al’s work on building a practical smartphone-based tool to accurately assess upper limb tremor in those suffering from Parkinson’s disease.
Associated with this tremor analysis trend has been a slew of studies that have looked at replacing expensive EMG readings with smartphone accelerometric readings.
Two years ago, a team of researchers at University of Coimbra showed that measurements from off-the-shelf apps, such as iSeismometer, could be used as a reliable alternative to EMG for tremor frequency assessment when it comes to the care of patients with a diagnosis of Parkinson’s, essential tremor and Holmes’ tremor.
This was followed by another study published last year, where accelerometric readings from an iPhone inserted into a patient’s socks could help detect orthostatic tremor. This is indeed a strong vindication of this approach, as orthostatic tremor was hitherto considered to be one of the few tremor conditions that required an EMG lab assessment for definitive diagnosis, given that leg tremors might not be visible to the naked eye.
Conclusion
On the concluding note, it is particularly impressive to note that, unlike similarly promising nexuses between gene editing and AI, for example, there is a far lesser degree of uncertainty and speculation here with noteworthy advancements already achieved that now await careful productisation.
The other two aspects that only enhance the prospects of this impending revolution of sorts are:
Emergence of deep learning as the computational framework of choice
Many of the results above have been achieved using simple (shallow) machine learning and traditional model-based signal processing approaches. As seen in the domains of speech, vision and text, deep learning has shattered state-of-the-art metrics by a fair distance. Given that adoption of deep learning-based approaches has been slow in the sensor domain, we will surely see the accuracies of these tests only go higher.
Sampling rates of sensors on phone
As things stand, motion sensor chips that are currently available in smartphones are severely underutilised in terms of the sampling rates these can provide. This is done mainly to extend battery life as well as on account of a few security concerns.
However, with the right security policies in place and use of specialised and well-monitored SDKs (such as Samsung health SDK), one can unlock the hidden potential of these nifty little workhorses, to open avenues for more granular and sensitive measurements at much higher sampling rates. This will, in turn, propel the way to more medical applications.
Vinay Uday Prabhu is principal machine learning scientist at UnifyID Inc., a security startup based in San Francisco, California. His current research lies at the intersection of deep learning, security and smartphone sensors. Prabhu holds a PhD in electrical and computer engineering from Carnegie Mellon University